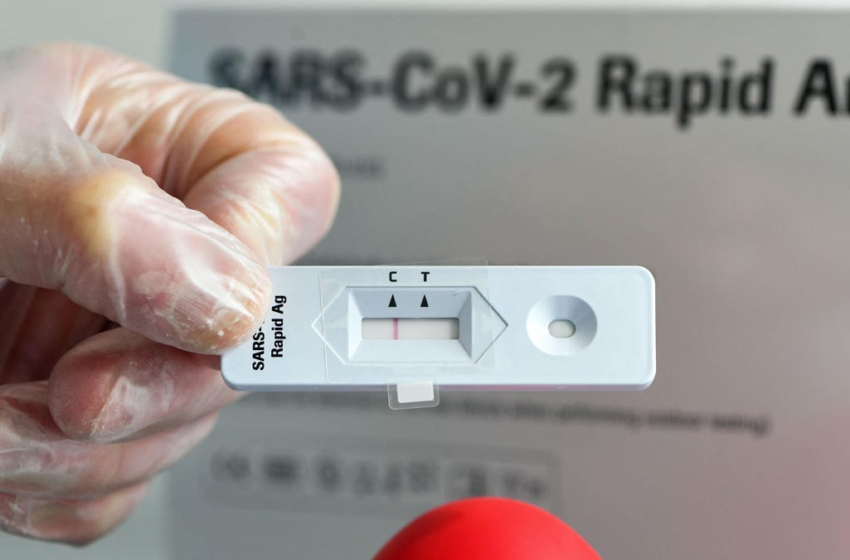
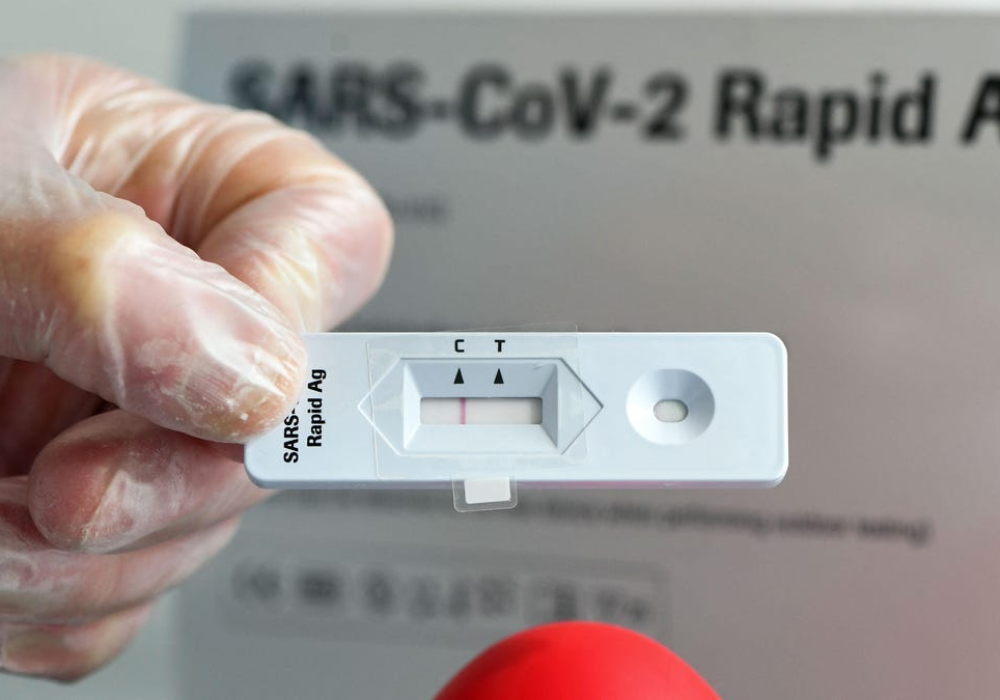
Health officials are warning that rapid covid-19 tests may be less accurate than before for people infected with the Omicron variant of the coronavirus. At least some antigen-based tests may have reduced specificity when testing for Omicron infections, the Food and Drug Administration reported this week, which could lead to a higher rate of false negative results. At this point, though, the FDA is still recommending that people use these tests as instructed.
The Omicron variant—first discovered in November—has quickly spread throughout the U.S. and world. Omicron has many more relevant mutations than previous forms of the coronavirus, which are allowing the variant to more easily infect people with prior immunity created through infection or vaccination. Typical cases of Omicron appear to be milder than those caused by Delta, the previously dominant variant, but it’s not yet clear how much of this relative mildness can be attributed to the virus itself or the high rates of population immunity. (In truth, it’s likely a mix of both.)
Omicron’s many mutations, though, have also raised the possibility that some tests designed to look for the virus could be more likely to fail, depending on the targets of the virus they use to verify infection. Anecdotally, there have been recent reports of people not testing positive despite clearly appearing to be sick. A previous FDA report found that while three molecular tests failed to detect omicron, there was no evidence that rapid antigen tests were less accurate. That conclusion has now changed.
On Tuesday, the FDA reported that a more recent lab analysis it conducted uncovered a potential problem with certain rapid tests. This newer analysis used live virus samples from patients, instead of heat-inactivated samples, which is thought to provide a better comparison to real world performance.
“Early data suggests that antigen tests do detect the omicron variant but may have reduced sensitivity,” the FDA said.
G/O Media may get a commission

20% Off
Select Nuraphone Styles
Get award-winning personalized sound
Grab the Nuratrue Earbuds, Nuraphone headphones, or the NuraLoop earbuds at a generous discount.
Specificity and sensitivity are the two indicators of accuracy for a diagnostic test, with sensitivity referring to the likelihood that any given positive result will be true. Tests with lower sensitivity are more likely to have false negatives, where someone with the diagnosed disease (covid-19 in this case) will mistakenly be told they don’t have it. In other words, someone with Omicron who takes an antigen test may be more likely to be wrongly reassured that they’re infection-free than if they had been infected with another variant.
For context, rapid antigen tests were already less sensitive than other types of covid-19 tests. This often amounted to people not testing positive for the virus as early as they would if they had taken a PCR test. But advocates of rapid tests argue that these tests are still quite excellent at detecting when someone is at the peak of their infection, and thus at their most contagious to others. Ideally, then, rapid tests should be used to protect others from being infected, not necessarily to let people know when they’ve become infected as soon as possible.
It doesn’t appear to be clear yet whether rapid tests will be any less effective at their intended goal for Omicron specifically. The FDA has said that it and other regulatory agencies are continuing to study how well rapid and other covid-19 tests are doing in the real world and if Omicron has changed things. For now, the agency is telling people to use rapid tests as instructed and follow the FDA’s current recommendations.
Those who test negative on a rapid test but still feel sick or suspect exposure to someone with covid-19, for instance, should get a follow-up molecular test (which will usually be PCR). Some countries and manufacturers also recommend that users take multiple rapid tests on successive days to better rule out the possibility of a false negative.