For decades, researchers have suspected that people infected with an exceedingly common virus, Epstein-Barr, might be more likely to develop multiple sclerosis, a neurological illness that affects a million people in the United States. Now, a team of researchers reports what some say is the most compelling evidence yet of a strong link between the two diseases.
The virus infects nearly everyone in their teen or young adult years, and very few go on to develop multiple sclerosis. The researchers also note that it is not the only known risk factor for people who develop the illness. But they say their data points to it being the clearest of them all. While it remains to be seen whether the finding will result in treatments or cures for multiple sclerosis, the study may further motivate research into therapies and vaccines for the condition.
In their study, published Thursday in Science, the group examined data from 10 million people on active duty in the United States Armed Forces over two decades. The strength of their study, said its principal investigator, Dr. Alberto Ascherio, an epidemiologist at the Harvard T.H. Chan School of Public Health, is that they were able to follow people for years and ask whether infections with Epstein-Barr preceded multiple sclerosis.
Among the service members in the study, 801 developed multiple sclerosis, a disabling disease that occurs when the immune system attacks the fatty insulation that protects nerves in the brain and spinal cord. Most who develop the disease are diagnosed between the ages of 20 and 50. The disease is rare, though — an individual’s chance of getting multiple sclerosis is half of one percent.
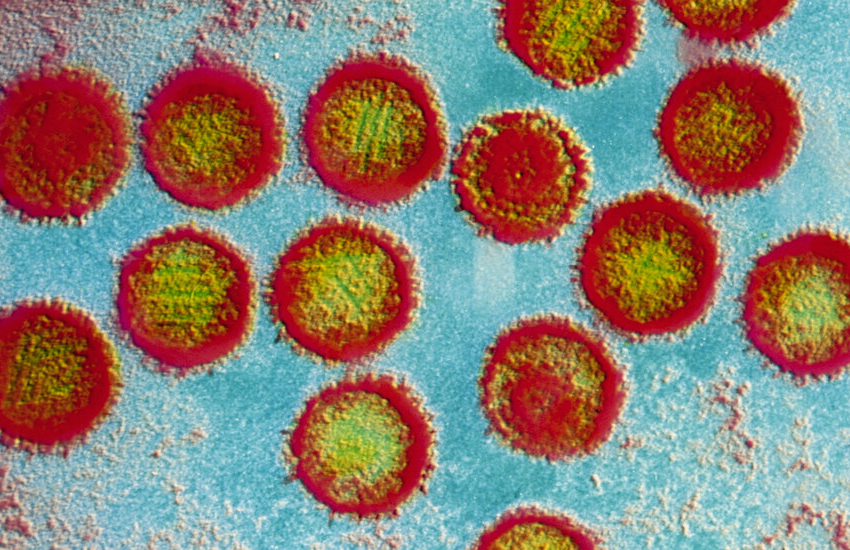
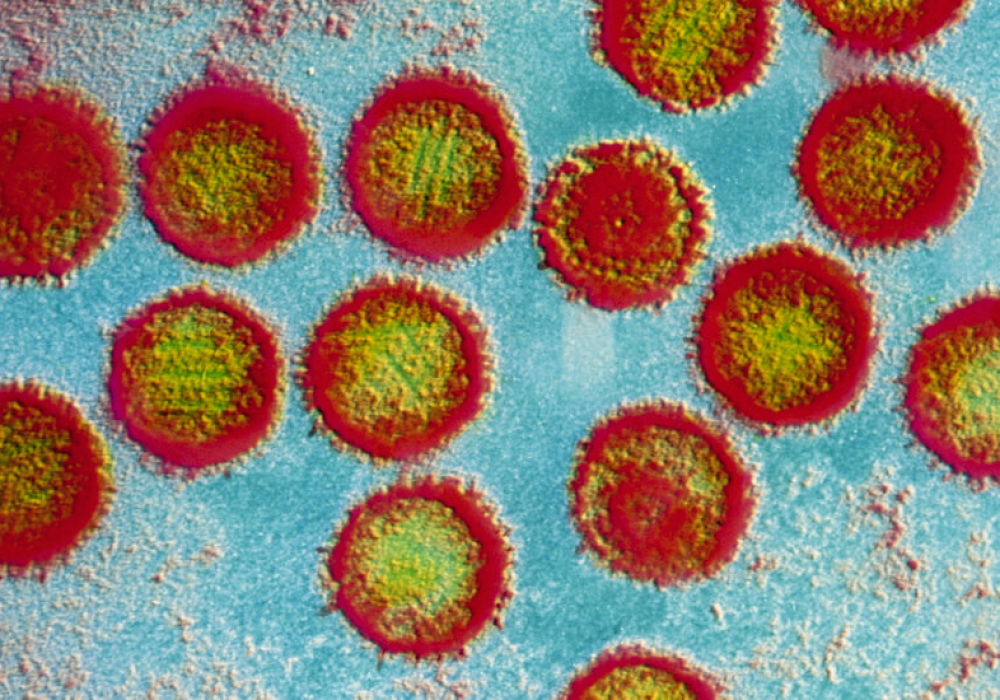
At the same time, the virus in question, Epstein-Barr, is common, infecting nearly everyone in the population at some point. Although few are aware that they were infected, some develop mononucleosis. The virus remains in the body for life.
Because so few who are infected with the virus get multiple sclerosis, it cannot be the sole cause of the disease. Other risk factors have been identified, including some, like low levels of vitamin D and smoking, that were seen previously by the Harvard group using the same data set. There also are genetic factors — 900 abnormal genes have been identified in patients with multiple sclerosis, said Dr. Anthony J. Reder, a multiple sclerosis expert at the University of Chicago, who was not involved in the new study. Gender also plays a role; most patients are women.
But, Dr. Ascherio said, no risk factor stands out like Epstein-Barr infections.
To ask how much the virus increases risk, the investigators studied the small proportion of people who were not infected with the virus early in their service careers but subsequently became infected. They detected infections by the presence of antibodies to the virus.
Among the multiple sclerosis patients, 32 out of 33 got infected with Epstein-Barr before they developed M.S.
As a control group for their study, the scientists tracked 90 individuals who were not initially infected with Epstein-Barr and who also did not get multiple sclerosis. Of them, just 51 subsequently became infected with Epstein-Barr.
That meant an Epstein-Barr virus infection increased the risk of multiple sclerosis over thirtyfold, Dr. Ascherio said.
But Dr. Reder cautioned that it could be hard to tease out cause and effect from an epidemiological study. People who develop multiple sclerosis have overactive immune systems that make them develop high levels of antibodies to viral infections. Multiple sclerosis might arise not because of the virus but because of the body’s response to it.
“Multiple sclerosis patients have fewer viral infections than normal,” he said, because their immune systems are so active that they effectively fight off viruses. “Multiple sclerosis patients often say, ‘I never get a cold.’ When I hear that, my ears perk up.”
The drugs currently used to treat multiple sclerosis suppress the immune system, Dr. Reder noted. So far, he added, anti-viral drugs have not helped patients with multiple sclerosis.
The Harvard group tried to control for the possibility that the immune system’s response, not the virus itself, increases the risk of multiple sclerosis in those infected with Epstein-Barr. They asked if antibodies to another common virus, cytomegalovirus, also were linked to a greater risk of multiple sclerosis. They were not.
But cytomegalovirus, Dr. Reder said, for unknown reasons, seems to protect against multiple sclerosis. So the fact that those infected with it did not have a higher risk of multiple sclerosis might not be surprising.
Others said the study was convincing evidence of cause and effect.
“The way it was done is quite compelling,” said Dr. Michael Davin Kornberg, a multiple sclerosis specialist at Johns Hopkins. “It really is the most convincing data we’ve had for a causal association.”
That leaves the question of what to do now.
Dr. Bruce Cree, a multiple sclerosis researcher at the University of California, San Francisco, noted that it might be difficult to treat multiple sclerosis by going after Epstein-Barr because it can be difficult to find the actual virus in patients. Even though multiple sclerosis is a disease of the brain and spinal cord, he could not find the virus in patients’ spinal fluid.
But patients do seem to harbor cells in their brains that produce antibodies to Epstein-Barr virus. Dr. Cree is researching whether he can treat multiple sclerosis patients by eradicating those cells, which are infected with Epstein-Barr.
And Dr. Lawrence Steinman, a multiple sclerosis researcher at Stanford, who wrote a perspective accompanying the Harvard group’s paper, said an experimental mRNA vaccine against Epstein-Barr was one of a number of approaches being designed to stop the virus from affecting the brain.
The question now, he said, is, “Can we make multiple sclerosis go away?”